Éloïse Gennet*
Junior Professor in law, Aix Marseille University, CNRS, DICE, CERIC, Aix-en-Provence, France

Aurélie Mahalatchimy
CNRS Permanent Researcher (CR) in law, Aix Marseille University, CNRS, DICE, CERIC, Aix-en-Provence, France
European Union law plays a great role in regulating “biomedical innovations” such as gene therapy, regenerative medicine or nanomedicine. Yet, the expression has been increasingly used in the literature and has emerged as a concept of science although not being homogenous. Considering it as a concept of legal science, we are defining biomedical innovation as an innovative product, procedure or technique based on biological elements of human or animal origin which entails high or unknown risks, and which serves a medical goal as well as economic competitiveness. Focusing on the biological component of biomedical innovations, and building on the characteristics of legally defined advanced therapy medicinal products, this paper explores if the biomedical innovation’s concept of legal science exists as a legal concept in applicable EU binding law, i.e. if EU law is considering, and/or defining biomedical innovations beyond the legal categories it embeds on the basis of identified and shared characteristics that would deserve to be regulated according to the EU legislator. Although it concludes that the expression “biomedical technologies” would better correspond to the EU legislator’s use, the analysis of EU binding law confirms the relevance of our definition of the biomedical innovation’s concept of legal science.
This work has been supported by ANR-funded I-BioLex project (ANR-20-CE26-0007-01).
* This work has been supported by the French government under the France 2030 program as part of the Aix‑Marseille University – A*MIDEX Excellence Initiative (AMX-22-CPJ-03) and by the ANR (N° ANR-22-CPJ2-0021-01).
Introduction
In the last decades, high hopes have been increasingly placed in biomedical innovations such as gene therapy, regenerative medicine or nanomedicine because of the promising potential they offer both for patients’ health and for EU’s market competitivity. European Union (EU) law plays a great role in regulating these types of innovations and make sure they can prosper yet without putting any patient at an unnecessary risk nor compromising major European values.1 In fact, those technologies evolve very quickly and although they are difficult to apprehend legally, the societal and health risks they inherently entail require close regulation.2 Yet the first step of any legal apprehension of a phenomenon, here the rise of biomedical innovations, is to determine its definition and scope.
Biomedical innovation appears as a scientific concept3 as well as a concept of legal science4 without being homogeneous.5 Indeed, it is often used without being defined precisely, especially in the field of intellectual property rights,6 and patents in particular,7 generally relating to biotechnology such as regarding ethics.8 It has also been used more specifically as relating to ‘biomodifying technology’,9 including stem cells.10
The initial starting point of this research was the specific case of advanced therapy medicinal products (ATMPs), which undoubtedly represent a good illustration of what we understand as being “biomedical innovations”. As formerly demonstrated,11 advanced therapy medicinal products (ATMPs), which have been legally defined in EU law,12 can be identified by five characteristics: they are developed with a medical goal in mind; they are innovative and/or include emerging technologies or processes; they are imprinted with uncertainties and unknown risks; the latent values and interests necessary for their development or regulation is ambiguous; and they might bring profound changes in their social, commercial or technological environment.
Our underlying hypothesis is that these characteristics of ATMPs may also be shared with other products or procedures based on biological elements of human or animal origin, such as in the fields of regenerative medicine, gene therapy or nanomedicine.13 Although neither these products or procedures nor these fields are legally defined in EU law, they all embed and overlap partially with each other.14 In order to explore legal framings of a set of biomedical innovations, without being limited to existing legal categories, such as ATMPs,15 we use ‘biomedical innovation’ as a concept of legal science.
Hence, we developed a hypothetical definition of biomedical innovation drawing on the characteristics of ATMPs. A biomedical innovation would be defined as an innovative product, procedure or technique based on biological elements of human or animal origin which entails high or unknow risks, and which serves a medical goal as well as economic competitiveness.16
In this paper, we want to explore the existence as well as the relevance of biomedical innovation as a legal concept in EU positive law. However, EU binding law does not itself use, let alone define, “biomedical innovations” per se, but only uses close expressions overlapping with what we consider as being included in the scientific concept of “biomedical innovations”.
For instance, regulation 726/2004 refers to “therapeutically innovative medicinal products”.17 However, this rather refers to the general “therapeutic, scientific or technical innovation”18 of any medicinal product that an applicant wants to obtain a marketing authorisation for, not only the ones based on biological elements. Moreover, one can also find the expression “biotechnological invention”19 in the patentability directive 98/44. However, this expression is a lot narrower than what we expect to encompass in “biomedical innovations”, notably because of the meaning of the term “invention” which is defined only so as to determine patentability requirements20 for inventive steps that are susceptible of industrial application.21 Regulation 726/2004 uses the expression “high-technology medicinal products, particularly those derived from biotechnology”, which is directly related in the same provision to “the emergence of new therapies, such as gene therapy and associated cell therapies, and xenogenic somatic therapy”.22
Hence the term “technology” seems to include a wide range of techniques, procedures and processes used on biological materials. Interestingly, tissue engineering, which is included in our understanding of biomedical innovations, is explicitly designated as a biotechnology. It is also explicitly designated as belonging to the field of regenerative medicine.23
Last but not least, the newly adopted regulation 2021/2282 on health technology assessment (thereafter “HTA regulation”), referring to directive 2011/24/EU, defines “health technology” as “a medicinal product, a medical device or medical and surgical procedures as well as measures for disease prevention, diagnosis or treatment used in healthcare”.24 This expression is also very close to our understanding of biomedical innovations as it refers to the medical objective on the contrary to the notion of biotechnology as used in EU binding law. However, it is still not appropriate as it would include all medical innovations, and not specifically biomedical innovations as the notion of health technology is not restricted to technologies including biological elements of human or animal origin but could also very well include digital technologies.25
In this paper, we want to confront our tentative definition of biomedical innovations with EU legally binding texts. We want to infer the key features of the definition of biomedical innovations from EU binding instruments when they formulate provisions that inform, directly or indirectly, on what could be a legal concept of “biomedical innovation”. In determining whether biomedical innovations share some, or all, of the identified characteristics and/or if other defining elements could be inferred from EU binding law, this paper will explore the potential emergence of a legal concept of biomedical innovation in EU binding law. This exploration and confrontation will permit to highlight potential links and differences between our concept of legal science and a potential legal concept26 in EU law on biomedical innovation, and possibly to alter, validate or complement our initial hypothetical definition.
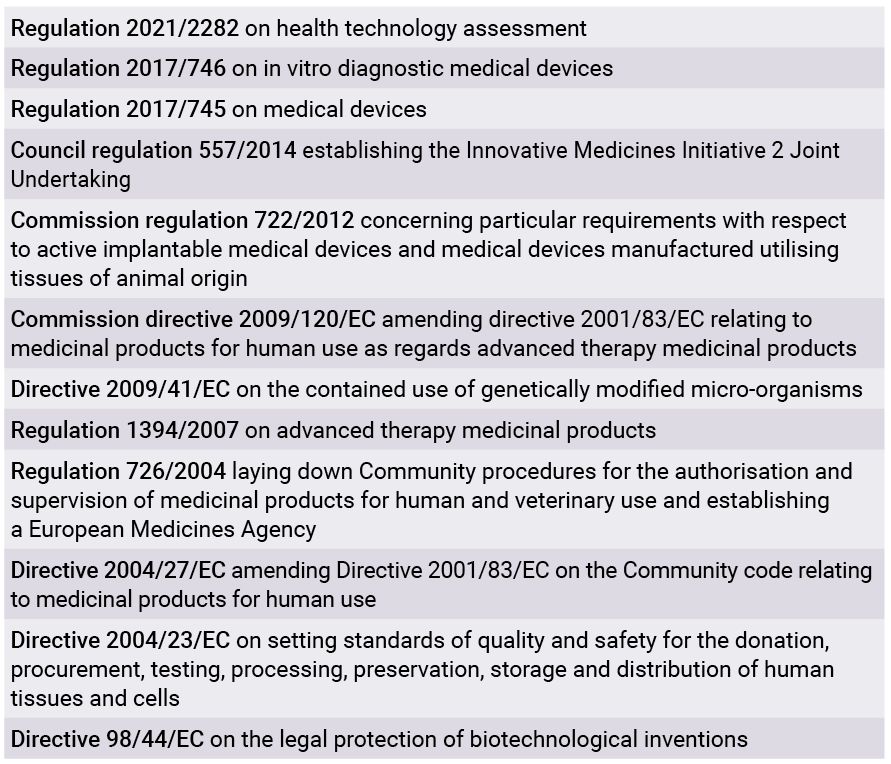
The selection criteria of the EU binding instruments applicable to biomedical innovations were broad: any currently binding law applicable to a specific innovation or group of innovations (for instance advanced therapy medicinal products, orphan medicinal products, in vitro medical devices etc.), but also any binding law potentially applicable to a biomedical innovation during parts or whole of its lifecycle (fundamental research, clinical research, commercialisation, patentability, manufacturing and packaging, pricing and reimbursement, vigilance etc.). Only currently applicable binding EU law was selected for analysis, including relevant case-law. Any binding law outside of the law of the European Union (e.g. national laws or the law of the Council of Europe), but also any EU non-binding law (e.g. recommendations, communications, reports, impact assessments or working documents) were excluded.27
The analysis was conducted on currently applicable EU binding law texts adopted between January 1985 and December 2021. Selection and analysis were conducted in four steps.
Step 1: A total of 65 EU binding instruments in the fields of medicinal products, medical devices and biotechnologies were listed. When applicable and available, for each of these binding instruments, the initial proposal of the European Commission, including and especially its explanatory memorandum, were also collected for analysis. The total number of instruments and their related documents amounted to 109 texts.
Step 2: A first analysis was conducted of all those 109 documents. The analysis was aimed at selecting the instruments that were giving some indications, criteria or a definition of notions such as “innovation” or “biomedical innovation”, and of the following specific biomedical innovations: “gene therapy”, “regenerative medicine” or “nanomedicine”.
This first step has led to the selection of twelve relevant texts for further analysis (see Table 1).
Step 3: Lastly, a search of the relevant case law of the Court of Justice of the European Union was also conducted. Several cases were selected for their relevant content on specific biomedical innovations or aspects thereof: the 2011 Oliver Brüstle case,28 2014 the International stem cell corporation case,29 the 2018 Confédération Paysanne case.30
Step 4: To conduct the in-depth analysis of the selected binding instruments, several ideas drawn from the above-mentioned characteristics of ATMPs have been targeted. More precisely, four interests at stake of the EU legislator on biomedical innovations have been identified as indicative or defining elements, namely research and innovation, economics, medicine and public health as well as the ethics and human rights. Two other topics that are transversal to the previous four have also been a particular focus for the analysis: the increased or unknown risks related to the biomedical innovation and the potential social, technological or commercial changes it might trigger. Finally, one last important element that has been the object of scrutiny is the existence of a gap, either between a societal or technological evolution and the absence of norms applicable to this evolution, or between a newly created legal category and the (so far) absence of innovation qualifying to fit in it. Such a regulatory gap may respectively create legal uncertainty and/or heterogeneity of regulation between EU Member States or steer scientific research and development towards giving an actual existence to the new category.
In the following developments, we will explain in a first part how this analysis has confirmed the dual objective of biomedical innovations when they are regulated in EU binding law (I). In fact, even though the qualifying term “biomedical” suggests that those types of innovations have a medical purpose, it is very clear from the analysis of the relevant EU binding law that they usually have a double objective, one of them being a medical objective, the other one being a market competitiveness objective. In a second part, we will examine which challenges of biomedical innovations seem to be systematically targeted by the EU legislator. These recognised challenges to be addressed indicate what the EU legislator considers to be main characteristics of biomedical innovations. The results of this analysis show not only that some of these characteristics confirm our definition of biomedical innovations, but also extend this definition with new characteristics (II).
I. Confirming the dual objective of biomedical innovations
Biotechnologies in the field of medicine can be considered as “‘building blocks’ of science and of technological development, [and] hold out the promise of socially beneficial products”,31 both from a medical and economic point of view. As stated above, there is no explicit definition of “biomedical innovations” in EU law. Yet the objectives of biomedical innovations can be considered as defining elements, especially in the regulatory context where these objectives determine, or are determined by, the Treaty provision on which the legal instrument is based. Most selected binding texts relevant to biomedical innovations are based on article 114 TFUE, which can be interpreted as a sign that biomedical innovations serve economic / market competitiveness. As the European Union has for a long time only had a supporting competence in the field of public health,32 the fields of pharmaceuticals and biotechnologies have long been the object of EU law solely on the legal basis of Article 114 TFEU, i.e. on the legal basis of the “approximation of the provisions laid down by law, regulation or administrative action in Member States which have as their object the establishment and functioning of the internal market”. And indeed, as visible in Table 2, out of the twelve selected ones for their relevance regarding biomedical innovations, only three instruments are not based on the internal market basis. Yet most of these instruments somehow reflect the medical goal attached to biomedical technologies, some of them are even solely based on article 168 TFEU, which can be interpreted as a sign that biomedical innovations also serve a public health goal. Then again, the European Union does not have a general shared competence in the field of public health beyond its supportive competence, or only, from the adoption of the Lisbon Treaty, for the very specific and restrictive goal of “setting high standards of quality and safety for medicinal products and devices for medical use” (Article 168.4.c TFEU). Hence, it was more difficult for the EU legislator to elaborate binding instruments on this basis solely. Nevertheless, it should be highlighted that the ‘mainstreaming’ provision anchoring the transversal nature of health, “health in all policies” (current Article 168.1 TFEU), can be traced back within the Internal market legal basis of the EU Treaty from 1996, the year of adoption of the Single European Act.33 As we will show, both the analysis of legal basis and of the content of the selected EU legally binding instruments regulating biomedical innovations have shown that they pursue this double objective most of the time. It is easily demonstrable with instruments having the double legal basis (B), but this can also be demonstrated with the content analysis of other instruments having none of both (A), or only one of them (C), with some exceptions.

Legal basis marked by a X. Colored in grey: objective revealed by the content analysis.
A) A double objective reflected in the instruments’ content only
Two of the studied instruments, although they are not based on article 114 TFEU nor on article 168 TFEU, still reflect this double objective of promoting EU’s economic competitiveness as well as protecting public health or health safety.
In fact, Council Regulation (EU) No 557/2014 establishing the Innovative Medicines Initiative 2 Joint Undertaking is based on articles 187 and 188 TFEU (Execution of Union research, technological development and demonstration programmes). Besides, the underlying economic objectives can be deducted from the content of its provisions although the instrument is also not based on article 114 TFEU. A first clue had already been given in the explanatory memorandum leading to regulation 557/2014, explaining that this Joint Undertaking was needed to “safeguard the future international competitiveness of the European biopharmaceutical and life-science industries such as diagnostics, vaccines, biomedical imaging and medical information technologies”,34 particularly in the general context of the “economic and financial crisis” and Europe’s need “to find a path to sustainable growth”.35 But even the instrument itself exposes its objectives, some of them being “to support [. . .] the development and implementation of pre-competitive research and of innovation activities of strategic importance to the Union’s competitiveness and industrial leadership or to address specific societal challenges [. . .] in particular the challenge to improve European citizens’ health and well-being”.36 This last quote thus also accounts for the underlying medical goal of this same regulation, which could also be easily deduced from the very title referring to innovative medicines. The goal of regulation 557/2014 is to involve a very broad range of partners and sectors in innovative therapies “to advance the development of new approaches and technologies for the prevention, diagnosis and treatment of diseases with high impact on public health”.37 Besides, it also states that innovative therapies should aim at priority medicines and/or new therapies for diseases for which there is a high unmet need but limited market incentives.38 Hence although the regulation is not based on article 168 TFEU, it is without doubt possible to deduce its objectives to promote health.
The second instrument that is neither legally based on public health nor on the internal market is Directive 2009/41/EC on the contained use of genetically modified micro-organisms, which is based on article 192 TFEU, i.e. the environment legal foundation. According to this provision, EU action relating to the environment “must be based on the principle that preventive action is to be taken and must have as its objective, among other things, the preservation, protection and improvement of the environment and the protection of human health”.39 Hence the protection of human health is already underlying in the action aiming at preserving or protecting the environment, as is indeed stated in the very first article of directive 2009/41.40 It is up to Member States to ensure appropriate measures are in place to avoid adverse effects on human health, and it is up to the user to carry out a risk assessment of the contained use.41 Finally, although it is not based on the internal market basis, Directive 2009/41 clearly states among its first recitals that “the development of biotechnology is such as to contribute to the economic expansion of the Member States”,42 hence clearly confirming the other objective to promote the internal market.
For a while, having a double legal basis remained an exception to the general principle according to which the legal basis should be adequate, adapted to the objectives of the instrument.43 The fact that more binding texts are based on the internal market rather than on public health is to be linked to the more important powers that article 114 TFEU gives to the legislator compared with 168 TFEU. Hence, this should not be interpreted as biomedical innovations’ objectives being predominantly directed towards economic competitiveness over the protection of health. Yet since the adoption of the Lisbon Treaty, and more precisely during the adoption process, the recourse to the double legal basis has suddenly become the preferred and systematic choice.44
B) A double objective reflected in the double legal basis
Four of the studied instruments have a co-legal basis reflecting this double objective. This is the case of regulation 726/2004 laying down Community procedures for the authorisation and supervision of medicinal products for human and veterinary use and establishing a European Medicines Agency, regulation (EU) 2017/745 on medical devices, regulation (EU) 2017/746 on in vitro diagnostic medical devices and of regulation (EU) 2021/2282 on health technology assessment, all based concomitantly on articles 114 TFEU and 168 TFEU.
Understandably, regulation 2017/745 puts forward the objectives of supporting harmonisation of legislation regarding medical devices in order to allow “rapid and cost-efficient market access for innovative medical devices, to the benefit of patients and healthcare professionals”.45 Similarly, the objectives of regulation 2017/746 clearly include the will to harmonise rules for small and medium enterprise who constitute 90% of the sector of in vitro diagnostic medical devices.46 Yet in the same way, both of these regulations also organize the safety risk evaluation of such devices,47 and permit, on grounds of public health and patient safety, to “take all appropriate measures to prohibit or restrict the device’s being made available on its national market, to withdraw the device from that market or to recall it until the manufacturer cooperates or provides complete and correct information”.48 This is part of the negative integration of public health in the establishment of the internal market.49
As for the HTA regulation on health technology assessment, market competitiveness objectives are stated right at the very first recital which states that “the development of health technologies is a key driver of economic growth and innovation in the Union” and that “health technologies constitute an innovative sector of the economy and form part of an overall market for healthcare expenditure that accounts for 10 % of Union gross domestic product [. . .]”.50 Of course, it also clearly states that the development of health technologies is “key to achieving the high level of health protection that health policies need to ensure for the benefit of all”.51 In fact, the regulation states that “HTA is able to contribute to the promotion of innovation, which offers the best outcomes for patients and society as a whole, and is an important tool for ensuring proper application and use of health technologies”,52 including warning when a technology becomes obsolete or assisting in the establishment of pricing and reimbursement at national levels. As a conclusion, it clearly appears from the content of the HTA regulation that a health technology has first and foremost a medical objective, yet the means to promote this medical objective lies primarily in the stimulation of innovation on the internal market.53 This is clearly reflected in the double legal basis of the regulation, but this is also the case for other EU binding instruments applicable to biomedical innovations despite those having only one legal basis.
C) A double objective despite a single legal basis ?
Most of the time, we can also find both objectives in the content analysis of the binding instruments, even though only one of them might be the actual legal basis. In fact, five out of the twelve binding texts54 have article 114 TFUE as a sole legal basis. However, this in itself does not exclude for those texts to also serve a medical goal. Health safety cannot be the primary objective under this legal basis, yet it remains an obligation. Article 114.3 TFEU indeed states that the Commission shall take as a base a “high level of protection”, notably concerning health safety and “taking account in particular of any new development based on scientific facts”. We will take two examples.
To begin with, directive 98/44 highlights in its first recital how much of a crucial role biotechnology and genetic engineering play in various industries and thus in Europe’s industrial development.55 Through “effective and harmonized protection”, the EU legislator hopes to “maintain and encourage investment in the field of biotechnology”.56 And in fact, as stated in the initial proposal of 1988 which led to the directive, the patent system is meant to “promote technical innovation as the major factor of economic growth by encouraging inventive activity through rewarding inventors for their creative efforts”.57 Yet besides this obvious economic objective, the crucial medical potential of biotechnological inventions is very clearly stated in the recitals of directive 98/44, saying that “development of biotechnology is important to developing countries, both in the field of health and combating major epidemics and endemic diseases and in that of combating hunger in the world” and that the patent system should thus be used to encourage research to meet the needs of Third World or of rare diseases.58 Even if it is not the primary goal, nor the goal of all biotechnological inventions, health protection and promotion remain potential underlying objectives that the EU legislator accounted for.
Next, ATMP regulation is also solely based on article 114 TFUE and thus directed at the promotion of the internal market. This regulation has been elaborated because the regulatory gap that was growing regarding Tissue engineered products, and leading to divergences between Member States in the authorization of ATMPs, and thus to the impairment of their free movement in the EU and of patients’ access.59 Thus, according to the explanatory memorandum accompanying the initial proposal that led to ATMP regulation, two of the four explicitly identified objectives of the regulation were on the one hand “to harmonise market access and to improve the functioning of the internal market by establishing a tailored and comprehensive regulatory framework for the authorisation, supervision and post-authorisation vigilance of advanced therapy products” and on the other hand “to foster the competitiveness of European undertakings operating in this field”.60 Yet, ATMPs are considered as medicinal products and thus inherently serve a medical goal.61 Hence another of these objectives was also to foster and frame the medical potential of advanced therapy medicinal products: “The advancement of science in the fields of biology, biotechnology and medicine, has fuelled the development of promising gene- and cell-based approaches for the prevention and treatment of diseases or dysfunctions of the human body. [. . .] In addition, a new biotechnology area has emerged: tissue engineering, which combines various aspects of medicine, cell and molecular biology, materials science and engineering, for the purpose of regenerating, repairing or replacing human tissues. [. . .] These three kinds of advanced therapies (gene therapy, somatic cell therapy, and tissue engineering) are expected to have a major impact on public health, by improving the quality of life of patients and changing medical practice significantly”.62
On the contrary to these illustrations, for some legally binding instruments in the field of biomedical technologies which have a single legal basis, internal market or public health, the content analysis did not allow to reveal an underlying second objective. This is the case of directive 2004/23. Directive 2004/23 on tissues and cells, has solely been based on ex article 152.4.a TEC, which permits to adopt measures “setting high standards of quality and safety” for “organs and substances of human origin, blood and blood derivatives” (now 168.4.a TFEU). In fact, “the transplantation of human tissues and cells is a strongly expanding field of medicine offering great opportunities for the treatment of as yet incurable diseases. The quality and safety of these substances should be ensured, particularly in order to prevent the transmission of diseases”,63 especially regarding current intensive exchanges around the globe.64
However, this exception can also be put into perspective as it is undeniable that guaranteeing a high level of quality and safety of tissues and cells can only be favourable to the free movement thereof on the internal market. Hence, this specific text does not prevent from concluding that the analysis of EU binding law confirmed that the latter considers as biomedical technologies procedures, processes or techniques based on biological elements of human or animal origin and that have a double objective: protecting or promoting health and improving market competitiveness.
Now in the following part, we will examine how EU binding law is regulating these biomedical technologies by identifying the challenges it is systematically targeting, thus hinting at what might be considered as the other key elements defining biomedical innovations.
II. Extending the characteristics of biomedical innovations
The way in which biomedical technologies are regulated in EU law is indicative of some of their characteristics. Defining elements of biomedical innovations can be inferred from the challenges that the EU legislator systematically has to face when regulating such innovations. Hence any identified feature can inform our attempt definition of a concept of legal science of biomedical innovations by providing important defining elements. And in fact, the analysis has revealed four challenges that may well be considered as an exhaustive list of defining characteristics of biomedical innovations. Two of them confirmed already identified features of our initial definition (A). Two others were less expected and thus have provided additional precisions that can be used to complement our proposed definition of a concept of legal science of biomedical innovations (B).
A) Characteristics confirming the proposed definition
Even if it is less obvious with the expression “biomedical technology” than “biomedical innovation”, the innovative character has been a central element considered by EU law. Indeed, the innovative dimension creates regulatory gaps which EU binding law is trying to bridge. More specifically, the EU legislator has considered that rapidly evolving innovative technologies require to adapt the legal framework to make sure they can circulate on the internal market (1). However, such adaptation has to take into account other challenges of biomedical technologies as considered under EU binding law: their inherent risks to human health, whether they are known or unknown (2). Doing so, EU binding law is confirming both the “innovative” characteristic and the high risks of biomedical technologies as highlighted in our definition of the biomedical innovations’ concept of legal science.
1) Rapidly evolving technologies
Several EU instruments often mention the fast pace of biomedical innovations. For instance, directive 2004/23 mentions the “rapid advance in biotechnology knowledge and practice in the field of human tissues and cells”.65 The explanatory memorandum that led to the ATMP regulation also recognizes on multiple occasions that the advanced therapies sector is “fast-growing” and “fast-evolving”66 because ATMPs “are based on complex, highly innovative manufacturing processes” and evolve in a sector (biotechnology, medical devices and pharmaceuticals) that is “subject to rapid and often radical innovation”.67
This fast pace and high complexity of the development of biomedical innovations creates regulatory gaps. There can for instance be a gap in the regulation of biomedical innovations between the phase of theoretical science uncovering a new scientific development and its successful transfer to applied sciences for it to actually become an innovation. This is what directive 98/44 was, in part, trying to answer with its patent system, aimed to encourage “inventive activity through rewarding inventors for their creative efforts”. More precisely in the field of biotechnology, the goal is to fill the “small and diminishing [. . .] gap between developments in basic science and their research and development applications”.68 The complexity and novelty of biomedical innovations thus often create regulatory gaps between the different phases of research and development, between the acknowledgment of a potential innovation and its concretization into a biomedical technology.
Even more pragmatically, and without even thinking yet about how this impacts innovation in general, this fast pace creates regulatory gaps at the most basic stages of scientific and technical requirements, even in already established domains of EU binding law. This is actually clearly accounted for by EU binding law about ATMPs. Only two years after the adoption of ATMP regulation, the EU legislator was already adopting directive 2009/120, acknowledging the “scientific and technical progress in the field of advanced therapies” and the resulting need to constantly update scientific and technical requirements accordingly.69
In fact, the new or rapid emergence of an innovation can, notably because of the differences of regulatory frameworks in EU Member States, cause a regulatory gap. Such regulatory gaps sometimes constitute an obstacle to the free flow of biomedical innovations and thus to research and innovation in general as well as to EU’s market competitiveness.
This was clearly visible in the preparation phase70 and then directly in the text of directive 98/44 about biotechnological inventions explaining that the different laws and practices of Member States “could create barriers to trade and hence impede the proper functioning of the internal market”, which “could lead to further disincentives to trade, to the detriment of the industrial development of such inventions and of the smooth operation of the internal market” .71
The recent HTA Regulation mentions for instance the complexity of the submission procedure and significant administrative burden for health technologies, resulting in a negative effect on innovation.72
Similarly, the ATMP regulation had been adopted with several objectives in mind, including to fill in a regulatory gap in the field of tissue engineered products regarding internal market and competitiveness as it notably formulates the objective “to provide overall legal certainty, while allowing for sufficient flexibility at technical level, in order to keep the pace with the evolution of science and technology”.73 Interestingly, the explanatory memorandum of its proposal also clearly exposes the impact on public health caused by the regulatory gap stemming from the incomplete regulatory picture for advanced therapies, notably because of the absence of regulation of tissue engineered products: “This leads to divergent, national approaches as to their legal classification and authorisation, thereby impairing the free movement of tissue engineered products in the Community, and hindering patients’ access to these innovative therapies”.74 Although the regulatory gap designated here targets the free movement on the EU market, it also hints at the particular risks to human health posed by biomedical innovations.
2) Technologies presenting inherent risks to human health
The presence of increased or unknown risks to human health (or to the environment) seems indeed to constitute an omnipresent element in the EU binding law applicable to biomedical innovations. For instance, the two consecutive regulations on medical devices, regulation 2017/745 and regulation 2017/746, result from the observation that “constant scientific and technological progress”75 can lead to “substantial divergences in the interpretation and application of the rules [. . .], thus undermining the main objectives of the Directives, i.e. the safety of medical devices and their free movement within the internal market”.76 When not taken into account at EU level, this regulatory gap on the risks to human health endangers European citizens when they benefit from a biomedical innovation in another EU country. Another example is also directive 2004/23, which “attempts to close the existing gap in Community legislation related to ensuring a high level of quality and safety of human tissues and cells” .77 It “seeks to ensure a comparable level of quality and safety of human tissues and cells in all Member States, bearing in mind the freedom of movement of citizens within Community territory”78 and the need to “facilitate exchanges thereof for patients receiving this type of therapy each year” thus ensuring a comparable quality and safety.79
The intention to close a regulatory gap in order to protect human health can be observed for all the selected instruments adopted on the legal basis of article 114.3 TFEU regarding the protection of a high level of health safety when regulating the internal market; and/or on the legal basis of public health as the latter is precisely directed towards high standards of safety of organs, blood, substances of human origin, medicinal products and medical devices (Art 168.4)a & c TFEU). But it is also the case of instruments with another legal basis. For instance, directive 2009/41 observes that genetically modified micro-organisms released into the environment may cross national frontiers, and therefore, “in order to bring about the safe development of biotechnology throughout the Community, it is necessary to establish common measures for the evaluation and reduction of the potential risks arising in the course of all operations involving the contained use of GMMs and to set appropriate conditions of use”.80
Many risks can be unknown, and this may be the concern expressed by the EU legislator when noticing the fact that the instrument is about a rapidly evolving field. For instance, directive 2004/23 mentions the need to adapt legal provisions “in light of the rapid advance in biotechnology knowledge and practice in the field of human tissues and cells”.81 The explanatory memorandum of the proposal for what became later the ATMP regulation also recognizes that advanced therapies sector often results from “not-yet-well-established processes and technologies”.82
However, some binding rules on the risks to human health from biomedical innovations actually target known risks that have realised in the past. For instance, regulation 722/2012 explicitly refers to the, then still relatively recent, mad cow disease and cites it as the reason for regulatory intervention, in order to update and apply the rules of directive 2003/32 to active implantable medical devices manufactured utilising tissues of animal origin in order to “maintain a high level of safety and health protection against the risk of transmitting animal spongiform encephalopathies to patients or other persons via medical devices manufactured utilising non-viable animal tissues or derivatives rendered non-viable”.83
Besides, these risks to human health can also be known, and be known to be increased. The uncertainty then is rather related to how much these risks are increased, hence the need for regulatory intervention. In that sense for instance, the explanatory memorandum of the proposal for what became later the ATMP regulation, notes that risks might be increased because ATMPs “can stay in the human body for a longer time than ‘conventional’ medicines”.84 The HTA regulation also acknowledges that, as risks can be increased at different levels, Member States should be able to undertake voluntary cooperation on HTA on medical devices / in vitro MD above a certain level of risk.85
However, although regulating on increased or uncertain risks is definitely a concern for the EU legislator in the field of biomedical innovations, it is difficult, from the EU binding texts only, to clearly identify whether the apprehension of these risks related to biomedical innovations really differs from the one of any medical device or medicinal product. In fact, the adoption of a classification by level of risk is now a common practice for medical devices86 or clinical trials of medicinal products,87 or even genetically modified micro-organisms,88 which then again corresponds too to the EU legal competency as formulated in Article 168(4)c TFEU.
Beyond the confirmation of the “innovative” characteristic and of the high risks of biomedical technologies as two defining elements of our biomedical innovations’ concept of legal science, EU binding law also provides some useful additional characteristics.
B) Additional characteristics for the proposed definition
When regulating biomedical technologies, the EU legislator has systematically recognized the importance of the ethical concerns (1) and public trust issues they raise (2). These are additional defining characteristics of biomedical technologies under EU binding law that can further inform the definition of biomedical innovations as a concept of legal science.
1) Technologies raising ethical concerns
The fact that biomedical technologies are based on biological elements of human origin inevitably leads to the consideration of ethics or human rights aspects in the EU binding instruments. The EU legislator sometimes has been explicit about his intention to close an inevitable regulatory gap in ethical questions, notably about biotechnological inventions for which he explains that “the most important thing is to assess the ethical dimension of certain biotechnological inventions which, unless otherwise clarified by the legislature, could turn out to be a Pandora’s box from which emotive issues are constantly likely to emerge”.89 Early on, directive 98/44 explicitly took position on ethical issues after following the European Group on Ethics in Sciences and New Technologies’ (thereafter “European Group on Ethics”) opinion:90 “Inventions shall be considered unpatentable where their commercial exploitation would be contrary to ordre public or morality”, hence the cloning of human beings or the industrial or commercial use of human embryos are considered unpatentable, as explicitly mentioned examples.91 Underlying this position is the idea that “patent law must be applied so as to respect the fundamental principles safeguarding the dignity and integrity of the person”.92
In fact, as we will see, the EU legislator will then take some distance with ethics principles or instruments and prefer referring to fundamental rights in its binding instruments applicable to biomedical innovations. These references are not systematic, nor always consistent and coherent with previous provisions, notably when it comes to mentioning the Convention on Human Rights and Biomedicine (Oviedo Convention)93 or the European Convention on Human Rights (ECHR)94 from the Council of Europe. In fact, recital 43 of directive 98/44 recalls that the EU respects fundamental rights as guaranteed by the ECHR. It does not mention the Oviedo Convention which was then open for signature but only entered into force in December 1999. However, both directive 2004/23 (recital 22) and the ATMP regulation (recital 8) directly refer to both the Charter of Fundamental Rights of the EU and the Oviedo Convention. Similarly, those three instruments all include a reference to previous or future work of the European Group on Ethics, at multiple occasions in directive 98/44,95 in directive 2004/2396 or in the ATMP regulation.97 On the contrary, more recent legally binding instruments on biomedical innovations, such as regulation 2017/745 and regulation 2017/746 only mention the Charter of Fundamental Rights of the EU (both in their recital 89), thus losing any reference to the Oviedo convention and to the work of the European Group on Ethics.
These inconsistencies of references to the Council of Europe’s instruments might be attributed to the adoption by the European Union of its own human rights instrument, the Charter of Fundamental Rights of the EU,98 which importance and authority has gradually evolved to become legally binding in 2009 with the coming into force of the Treaty of Lisbon. EU binding law instruments thus contain provisions related to the requirement to obtain the free and informed consent of the person from whom biological elements are taken, for instance directive 98/44,99 directive 2004/23,100 later even with specific requirements for incapacitated minors, pregnant and breastfeeding women, persons deprived of liberty and patients in emergency situations as in both regulations on medical devices, regulation 2017/745 and regulation 2017/746.101 Besides, some of these instruments, notably directive 2004/23, regulation 2017/745 and regulation 2017/746, also include provisions on confidentiality and data protection, notably when it contains personal data from the human biological elements.102
The absence of any further reference to the work and opinion of the European Group on Ethics shows how careful the EU legislator is with ethical issues, since it predominantly remains a sovereignty field of national laws. Interestingly, the EU legislator has sometimes used the pretext of being competent to regulate health and safety issues of biomedical technologies to take position on ethical questions. It has done so, in several instruments, about the principle of voluntary and unpaid donation and the fact that it “may contribute to high safety standards for tissues and cells and therefore to the protection of human health”.103
In fact, during the legislative process leading to the adoption of directive 2004/23, parliamentary amendments had tried to add “extensive ethical provisions” that the Commission explicitly recognized as legitimate and to which she gave “careful consideration”, but only accepted those related to the anonymity of donors and/or non-profit procurement. Other amendments were deemed outside the scope of Article 152 (now 168 TFUE) on public health provisions, because this article does not aim for ethical objectives to be implemented as such.104 For instance, it will not interfere on such topics like the use or non-use of human germ cells or embryonic stem cells, yet if the latter was authorized in a Member State, “this Directive will require the application of all provisions necessary to protect public health, given the specific risks of these cells based on the scientific knowledge and their particular nature, and guarantee respect for fundamental rights”.105 As the EU legislator considers that “voluntary and unpaid tissue and cell donations are a factor which may contribute to high safety standards for tissues and cells and therefore to the protection of human health”, it harmonizes, via Article 12 of directive 2004/23, aspects that are also directly relevant to human rights and ethical norms like compensation, “which is strictly limited to making good the expenses and inconveniences related to the donation”,106 or the rule that procurement and tissues and cells is carried out “on a non-profit basis”.107 We can find another example in the ATMP regulation,108 which also touches upon anonymous, voluntary and unpaid donation of human cells and tissues contained in advanced therapy medicinal products, as it “may contribute to high safety standards for cells and tissues and therefore to the protection of human health”.109 Interestingly, it also adds that “altruism of the donor and solidarity between donor and recipient should be respected”.110
Hence, it is clearly visible that biomedical technologies raise human rights issues that are handled in different EU binding instruments. Although biomedical technologies clearly also raise ethical issues, the EU legislators show more prudence and now avoids any explicit ethical reference, even where ethics principles are clearly involved.
2) Technologies challenging public trust and confidence
The singular combination of how EU law regulates biomedical technologies and their identified characteristics also seems to justify the need for the EU legislator to seek public trust and confidence in these biomedical technologies. Indeed, we could also often find indicators of the recurring intention of the EU legislator “to preserve the confidence of patients and medical practitioners in their evaluation”,111 to “help to reassure the public”112 and “increase confidence among the Member States”113 or “ensuring a high level of health and safety protection and citizens’ confidence in the system which has come under severe criticism in recent years”.114 Some authors explain that since mad cow disease, trust in science has been declining in Europe: “the development of innovations in biotechnology has been hampered by this lack of trust due to public concerns about the adequacy of the regulatory process, its openness and transparency, and potential conflicts of interest arising from government, industry and university partnerships”.115 Nevertheless, the public confidence in science and technology has evolved positively, as shown by the 2021 Eurobarometer survey116 that appear as a potential indicator of the success of EU law on this aspect.
These efforts to gain public trust can be seen as part of a legitimation process of the EU legislation on biomedical technologies.117 It could also be explained by a proactive intention to speed up the adoption of biomedical technologies. In fact, innovations only become actual innovations when they are adopted by society, when involved stakeholders and citizens recognise it as such and embrace its use.118
Thus, this analysis is not only confirming the innovative and risky character of biomedical technologies as two relevant elements of the definition of our biomedical innovations’ concept of legal science, it also highlights that EU binding law considers two additional challenges of biomedical technologies when regulating them: the ethical concerns they raised as well as public trust in the field. As these additional challenges are common to all studied biomedical technologies, they become inherent characteristics that could be added in the proposed definition of biomedical innovations as a concept of legal science.
Conclusion
To sum up, we have shown that the concept of biomedical innovation is not explicitly used in EU binding law, i.e the denomination of the concept does not appear in EU binding law. Indeed, the content analysis of relevant instruments shows that our understanding of biomedical innovation is a subtype of health technologies as understood in the HTA regulation. Within these health technologies, biomedical technologies are products, procedures or techniques which are based on biological elements of human or animal origin and which have at least two parallel objectives: an economic objective and a medical objective.
The content analysis of relevant EU binding law instruments has also shown recurring issues that the EU legislator seems to encounter when regulating biomedical technologies. Their innovativeness, complexity and rapid evolution creates regulatory gaps requiring the intervention at the EU level to guarantee a continued circulation on the market but also to mitigate the high or uncertain risks that biomedical technologies often pose and to make sure to protect fundamental rights as well as to seek public trust and confidence in the process of developing or administering those biomedical technologies. These recurring issues, that confirm but also extend our initial definition of biomedical innovations, may thus be considered as the main elements defining a legal concept of biomedical technologies.
1 A. Mahalatchimy, “La promotion de l’innovation en matière de santé: quelles logiques à l’œuvre dans l’Union européenne ?”, Revue des Affaires Européennes, May 2018, 2017/4, pp. 627-636.
2 A. Mahalatchimy, “Pour une stratégie de l’Union européenne dans le domaine de l’innovation en santé”, Revue de l’Union Européenne, January 2019, n° 624, pp. 22-29.
3 A scientific concept (of philosophy, medicine, sociology, etc.) “is used by a scientific discourse other than the one on the law”, Introduction, this dossier.
4 A concept of legal science “is used in scholarly discourse on the law”, Introduction, this dossier.
5 A quick search on the expression “biomedical innovation” on the database of the University of Aix-Marseille gives 4,946 results.
6 See for instance, J. de Beer, C. Brusnyk, “Intellectual property and biomedical innovation in the context of Canadian federalism”, Health Law Journal, 2011, vol. 19, pp. 45-82.
7 See for instance, J. P.Walsh, A. Arora, W.M. Cohen, “Effects of Research Tool Patents and Licensing on Biomedical Innovation”, in W. M. Cohen, S. A. Merrill (eds.), Patents in the Knowledge-Based Economy, National Academies Press, Washington, D.C., 2003, pp. 285-340.
8 K. R. Jongsma, A. L. Bredenoord, “Ethics parallel research: an approach for (early) ethical guidance of biomedical innovation”, BMC Med Ethics, September 2020, vol. 21, n° 1, p. 81.
9 E. Bicudo, M. Morrison, P. Li, A. Faulkner, A. Webster, M. Mourby, J. Kaye, “Patent power in biomedical innovation: technology governance in biomodifying technologies”, The Journal of World Intellectual Property, 2022, n° 25, pp. 473–494.
10 B. Salter, Y. Zhou, S. Datta, “Hegemony in the marketplace of biomedical innovation: Consumer demand and stem cell science”, Social Science & Medicine, 2015, vol. 131, pp. 156-163.
11 A. Mahalatchimy, L’impact du droit de l’Union européenne sur la règlementation des médicaments de thérapie innovante en France et au Royaume-Uni, Thèse de doctorat en droit public, Université Toulouse 1 Capitole, 2015, pp. 40-44 building on Nuffield Council on Bioethics, Emerging biotechnologies : technology, choice and the public good, December 2012.
12 Regulation (EC) No 1394/2007 of the European Parliament and of the Council of 13 November 2007 on advanced therapy medicinal products and amending Directive 2001/83/EC and Regulation (EC) No 726/2004 (Text with EEA relevance), OJ L 324, 10.12.2007, p. 121–137, CELEX number: 32007R1394, Article 2§ 1 a).
13 “BioGOV: Governing Biomodification in the Life Sciences” (2018-2022), research project funded by the Leverhulme Trust and led by Professor Jane Kaye (last access, 8th October 2024).
14 A. Mahalatchimy, L’impact du droit de l’Union européenne sur la règlementation des médicaments de thérapie innovante en France et au Royaume-Uni, op. cit. p. 28-40.
15 This is the object of the research project I-BioLex, op. cit.
16 “I-BioLex: Fragmentation and defragmentation of the law on biomedical innovations” (2021‑2025), research project funded by the French National Agency for Research and led by Dr Aurélie Mahalatchimy (last access, 8th October 2024).
17 Regulation (EC) No 726/2004 of the European Parliament and of the Council of 31 March 2004 laying down Community procedures for the authorisation and supervision of medicinal products for human and veterinary use and establishing a European Medicines Agency (Text with EEA relevance), OJ L 136, 30.4.2004, p. 1–33, CELEX number: 32004R0726, Recital 9.
18 Ibid., Article 3.b.
19 Directive 98/44/EC of the European Parliament and of the Council of 6 July 1998 on the legal protection of biotechnological inventions, OJ L 213, 30.7.1998, p. 13–21.
20 Directive 98/44/EC, op. cit., Expl memo, § 37.
21 “1. For the purposes of this Directive, inventions which are new, which involve an inventive step and which are susceptible of industrial application shall be patentable even if they concern a product consisting of or containing biological material or a process by means of which biological material is produced, processed or used; 2. Biological material which is isolated from its natural environment or produced by means of a technical process may be the subject of an invention even if it previously occurred in nature.” Ibid., Article 3.
22 Regulation (EC) No 726/2004, op. cit., Recital 7.
23 Judgment of the General Court (Ninth Chamber), 2 March 2022, VeriGraft AB v. European Innovation Council and SMEs Executive Agency, T‑688/19, ECLI:EU:T:2022:112.
24 Regulation (EU) 2021/2282 of the European Parliament and of the Council of 15 December 2021 on health technology assessment and amending Directive 2011/24/EU, OJ L 458, 22 December 2021, p. 1–32, CELEX number: 32021R2282, Article 2(4) (and in recital 1).
25 It is the case for instance of the OECD, which includes both biomedical and digital technologies in its definition of health technologies: “Health technology and innovation is defined as the application of knowledge to solve practical clinical and health problems, including products, procedures and practice styles that alter the way health care is delivered. Such a definition includes biomedical technology—such as medicines, medical devices and diagnostics (Dx)—as well as enabling technology such as mobile health (mHealth) and ‘Big Data’. [. . .].” OECD, New Health technologies, Managing Access, Value and Sustainability, DOI :10.1787/9789264266438, 2017, p. 18.
26 A legal concept “is contained in provisions of positive law (an applicable legal text whatever its source or status is (Act, Decree, …) at a given time in a given legal order)”, Introduction, this dossier.
27 The study of non-binding law relatively to complementary research questions was done in a second phase, and is the object of another paper in this dossier.
28 CJEU, 18 October 2011, Oliver Brüstle c/ Greenpeace eV, C-34/10, Rec. I-09821, ECLI:EU:C:2011:669.
29 CJEU, gr. ch., 18 December 2014, International Stem Cell Corporation c/ Comptroller General of Patents, C-364/13, ECLI:EU:C:2014:2451.
30 CJEU, gr. ch., 25 July 2018, Confédération paysanne and Others v. Premier ministre and Ministre de l’Agriculture, de l’Agroalimentaire et de la Forêt, C-528/16, ECLI:EU:C:2018:583.
31 O. Feeney, J. Cockbain, M. Morrison, et al., “Patenting Foundational Technologies: Lessons From CRISPR and Other Core Biotechnologies”, The American Journal of Bioethics, vol. 18, n° 12, 2018, p. 36.
32 N. De Grove-Valdeyron, Droit européen de la santé, 2nd edition, LGDJ, 2018.
33 T. K. Hervey and J. V. McHale (eds), European Union Health Law, Cambridge University Press, 2015, p. 62.
34 Council Regulation (EU) No 557/2014 of 6 May 2014 establishing the Innovative Medicines Initiative 2 Joint Undertaking (Text with EEA relevance), OJ L 169, 7.6.2014, p. 54–76, CELEX number: 32014R0557, Expl memo, § 1.
35 And especially so as “industry on its own will not invest due to these obstacles, and because public support from the Member States acting alone is too fragmented and cannot achieve the coordinated, long-term, large-scale, transnational, cross-sectorial effort required.” Ibid.
36 Full sentence: “to support, in accordance with Article 25 of Regulation (EU) No 1291/2013, the development and implementation of pre-competitive research and of innovation activities of strategic importance to the Union’s competitiveness and industrial leadership or to address specific societal challenges in particular as described in parts II and III of Annex I to Decision 2013/743/EU, and in particular the challenge to improve European citizens’ health and well-being.” Ibid., Article 2.a.
37 Ibid., Recital 8.
38 For instance, Alzheimer’s disease or antimicrobial resistance: Ibid., Article 2(a)(I) and (iii).
39 Directive 2009/41/EC of the European Parliament and of the Council of 6 May 2009 on the contained use of genetically modified micro-organisms (Recast) (Text with EEA relevance), OJ L 125, 21.5.2009, p. 75–97, CELEX number: 32009L0041, Recital 2.
40 It “lays down common measures for the contained use of genetically modified micro-organisms with a view to protecting human health and the environment.” Ibid., Article 1.
41 Ibid., Article 4.
42 Ibid., Recital 4.
43 For a thorough analysis thereof: A. Mahalatchimy, L’impact du droit de l’Union européenne sur la règlementation des médicaments de thérapie innovante en France et au Royaume- Uni, op. cit., p. 133.
44 Ibid., p. 136.
45 Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on medical devices, amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and repealing Council Directives 90/385/EEC and 93/42/EEC (Text with EEA relevance), OJ L 117, 5.5.2017, p. 1–175, CELEX number: 32017R0745, Expl memo, § 1.
46 Regulation (EU) 2017/746 of the European Parliament and of the Council of 5 April 2017 on in vitro diagnostic medical devices and repealing Directive 98/79/EC and Commission Decision 2010/227/EU (Text with EEA relevance), OJ L 117, 5.5.2017, p. 176–332, CELEX number: 32017R0746, Expl memo, § 3.1.
47 Regulation (EU) 2017/745, op. cit., Article 94; Regulation (EU) 2017/746, op. cit., Article 89.
48 Regulation (EU) 2017/745, op. cit., Article 10.14, see also article 98; Regulation (EU) 2017/746, op. cit., Article 93.
49 N. De Grove-Valdeyron, Droit européen de la santé, 2nd edition, LGDJ, 2018, p. 17.
50 Regulation (EU) 2021/2282, op. cit., Recital 1.
51 Ibid., Recital 1.
52 Ibid., Recital 3.
53 The goal is to help « creating and maintaining sustainable healthcare systems, and stimulate innovation that delivers better outcomes for patients ». Ibid., Recital 5.
54 Based on 114 TFUE only: Directive 98/44/EC, op. cit.; Regulation (EC) No 1394/2007, op. cit.; Commission Directive 2009/120/EC, op. cit.; Commission Regulation (EU) No 722/2012 of 8 August 2012 concerning particular requirements as regards the requirements laid down in Council Directives 90/385/EEC and 93/42/EEC with respect to active implantable medical devices and medical devices manufactured utilising tissues of animal origin (Text with EEA relevance), OJ L 212, 9.8.2012, p. 3–12, CELEX number: 32012R0722.
55 Directive 98/44/EC, op. cit., Recital 1.
56 Ibid., Recital 3.
57 Ibid., Expl memo, §I.A.2); citing: COM(88) 496 final – SYN 159, 17 October 1988; OJ No C 10, 13.1.1989, paragraph 11, p. 6. The proposal even describes the estimation in dollars of the world market for biotechnological products and how it had been refined and how it had grown even only since the publication of the first proposal for a directive, with detailed information and statistics/numbers depending on the type of industry and/or on the company and/or country. Ibid., §I.A.24); See as well in the same document the Annex p. 22: « Information on the industries using biotechnology ».
58 Directive 98/44/EC, op. cit., Recitals 11 and 18.
59 Regulation (EC) No 1394/2007, op. cit., Expl memo, § 1.
60 Ibid., § 2.1.
61 The explanatory memorandum also precises that tissue engineered products constitute medicinal products from a legal point of view, « for at least one of the following reasons:
– They are presented as having properties for treating or preventing disease in human beings;
– They are used in or administered to human beings with a view to restoring, correcting or modifying physiological functions by exerting a pharmacological, immunological or metabolic action;
– In accordance with the jurisprudence of the European Court of Justice (ECJ) on the matter, they are capable of having a significant effect on the actual functioning of the body ». Ibid., § 3.1.
62 Regulation (EC) No 1394/2007, op. cit., Expl memo, § 1 and § 2.1.
63 Directive 2004/23/EC of the European Parliament and of the Council of 31 March 2004 on setting standards of quality and safety for the donation, procurement, testing, processing, preservation, storage and distribution of human tissues and cells, OJ L 102, 7.4.2004, p. 48–58, CELEX number: 32004L0023, Recital 1, see also article 1.
64 Ibid., Recital 5.
65 Ibid., Recital 32.
66 Regulation (EC) No 1394/2007, op. cit., Expl memo, § 2.4.
67 Ibid., § 1.
68 Directive 98/44/EC, op. cit., Expl memo, § 1.
69 Commission Directive 2009/120/EC, op. cit., Recital 3).
70 “That uncertainty will hamper the free movement of biotechnological products and investment in research and development for new biotechnological products and processes.” Directive 98/44/EC, op. cit., Expl memo, § 7.
71 “Whereas differences exist in the legal protection of biotechnological inventions offered by the laws and practices of the different Member States; whereas such differences could create barriers to trade and hence impede the proper functioning of the internal market; Whereas such differences could well become greater as Member States adopt new and different legislation and administrative practices, or whereas national case-law interpreting such legislation develops differently; Whereas uncoordinated development of national laws on the legal protection of biotechnological inventions in the Community could lead to further disincentives to trade, to the detriment of the industrial development of such inventions and of the smooth operation of the internal market.” Directive 98/44/EC, op. cit., Recitals 5-7.
72 Regulation (EU) 2021/2282, op. cit., Recital 13.
73 Regulation (EC) No 1394/2007, op. cit., Expl memo, § 1.
74 Ibid.
75 Expl memo § 1 in both proposals that lead to Regulation (EU) 2017/745, op. cit., and Regulation (EU) 2017/746, op. cit.
76 Ibid.
77 Directive 2004/23, op. cit., Expl. Memo (B).
78 Ibid.
79 Directive 2004/23, op. cit., Recital 4.
80 Directive 2009/41/EC, op. cit., Recitals 7 and 8.
81 Directive 2004/23, op. cit., Recital 32.
82 Regulation (EC) No 1394/2007, op. cit., Expl memo, § 3.2.
83 Commission Regulation (EU) No 722/2012, op. cit., Recitals 2 and 5.
84 Regulation (EC) No 1394/2007, op. cit., Expl memo, § 3.4.
85 Regulation (EU) 2021/2282, op. cit., Recital 18.
86 For instance: Regulation (EU) 2017/745, op. cit., Article 51.
87 Notably with the new category of “low intervention clinical trials.” Regulation (EU) No 536/2014 of the European Parliament and of the Council of 16 April 2014 on clinical trials on medicinal products for human use, and repealing Directive 2001/20/EC Text with EEA relevance, OJ L 158, 27.5.2014, p. 1–76, CELEX number: 32014R0536, Recital 11 & article 2.2(3) & article 5.2.
88 Directive 2009/41/EC, op. cit., Article 4.3.
89 Directive 98/44/EC, op. cit., Expl memo, § 13.
90 Ibid., recitals 19 and 44, and articles 6 and 7.
91 Are unpatentable: “(a) processes for cloning human beings; (b) processes for modifying the germ line genetic identity of human beings; (c) uses of human embryos for industrial or commercial purposes; (d) processes for modifying the genetic identity of animals which are likely to cause them suffering without any substantial medical benefit to man or animal, and also animals resulting from such processes.” Ibid., Article 6.
92 And that “the human body, at any stage in its formation or development, including germ cells, and the simple discovery of one of its elements or one of its products, including the sequence or partial sequence of a human gene, cannot be patented.” Ibid., Recital 16.
93 Council of Europe, Convention for the protection of Human Rights and Dignity of the Human Being with regard to the Application of Biology and Medicine: Convention on Human Rights and Biomedicine, ETS No. 164, Oviedo, 4 April 1997.
94 Council of Europe, Convention for the Protection of Human Rights and Fundamental Freedoms, ETS No. 005, Rome, 4 November 1950.
95 Article 7: “The Commission’s European Group on Ethics in Science and New Technologies”; Recital 44 repeats article 7 and gives a precision: “whereas it should be pointed out in this connection that that Group may be consulted only where biotechnology is to be evaluated at the level of basic ethical principles, including where it is consulted on patent law”; Recital 19: “Whereas account has been taken of Opinion No 8 of the Group of Advisers on the Ethical Implications of Biotechnology to the European Commission.” Directive 98/44/EC, op. cit.
96 Directive 2004/23, op. cit., Recital 33 states: “The opinions of the Scientific Committee for Medicinal Products and Medical Devices and that of the European Group on Ethics in Science and New Technologies have been taken into account, as well as international experience in this field, and will be sought in the future whenever necessary.”
97 Regulation (EC) No 1394/2007, op. cit., Recital 28.
98 Charter of Fundamental Rights of the European Union, OJ C 326, 26.10.2012, p. 391–407.
99 It imposes that the person from whom biological material is taken and used in a patent application must have been given the “opportunity of expressing free and informed consent thereto, in accordance with national law.” Directive 98/44/EC, op. cit., Recital 26.
100 Directive 2004/23, op. cit., Article 13 & Annex.
101 Regulation (EU) 2017/745, op. cit., Articles 62-69; Regulation (EU) 2017/746, op. cit., Articles 59-64.
102 Directive 2004/23, op. cit., Article 14; Regulation (EU) 2017/745, op. cit., Articles 109-110; Regulation (EU) 2017/746, op. cit., Articles 102-103.
103 Directive 2004/23, op. cit., Recital 19.
104 Directive 2004/23, op. cit., Expl memo amended proposal 2004/23, §C.1.
105 Directive 2004/23, op. cit., Recital 12.
106 Ibid., Article 12.1.
107 Ibid., Article 12.2.
108 A. Mahalatchimy, “Bioethics and European Union: the Advanced Therapy Medicinal Products’ case”, Opinio Juris in Comparatione, vol. 2, n° 3, 2010.
109 Regulation (EC) No 1394/2007, op. cit., Recital 15.
110 Ibid., Recital 15.
111 Regulation (EC) No 1394/2007, op. cit., § 3.2; Regulation (EC) No 726/2004, op. cit., Recital 7.
112 Directive 2004/23 more explicitly describes an “urgent need for a unified framework in order to ensure high standards of quality and safety” of human tissues and cells, in order to “help to reassure the public.” Directive 2004/23, op. cit., Recital 4.
113 More precisely: “increase confidence among the Member States in the quality and safety of donated tissues and cells, in the health protection of living donors and respect for deceased donors and in the safety of the application process.” Directive 2004/23, op. cit., Recital 15.
114 Regulation (EU) 2017/745, op. cit., Expl memo, § 1; Regulation (EU) 2017/746, op. cit., Expl memo, § 1.
115 M. D. Mehta, “The Future of Nanomedicine Looks Promising, but Only If We Learn from the Past”, Health Law Review, vol. 13, n° 1, 2004, p. 17.
116 Eurobaromater survey, What Europeans think about science and technology?, 2021 (accessed on 2 March 2024).
117 A. Mahalatchimy, P. L. Lau, P. Li, M. Flear, “Framing and Legitimating EU Legal Regulation of Human Gene-Editing Technologies: Key Facets and Functions of an Imaginary”, Journal of Law and the Biosciences, vol. 8, n° 2, 2021, pp. 1-30.
118 V. Tournay, La gouvernance des innovations biomédicales. Vers une science politique pragmatique, PUF, Paris, 2007.
Éloïse Gennet, Aurélie Mahalatchimy, « Is there a legal concept of biomedical innovations in EU binding law? », Définitions et concepts du biodroit [Dossier], Confluence des droits_La revue [En ligne], 07 | 2025, mis en ligne le 7 juillet 2025. URL : https://confluencedesdroits-larevue.com/?p=4181.